Pain is a Big Thing to Pharmacists
Greetings from the American Pharmacists Association (APhA) meeting in Baltimore, Maryland! The APhA chose a really nice location for our Spring meeting this year. There was a definite hint of Spring in the first weekend of March.
I flew into Newport News, Virginia on Friday to attend the christening of a new nuclear submarine, the USS Washington, on which my son is serving, and then made my way to Baltimore.
Years ago, I came across what I thought would be one of the coolest jobs in the world: being a “cool hunter”. Cool hunters, as you might imagine, hunt for things that are cool, for what will be the next big fashion.
There are many talks, posters and exhibitors that make APhA a great place for “cool hunting” the big topics in pharmacy and patient care.
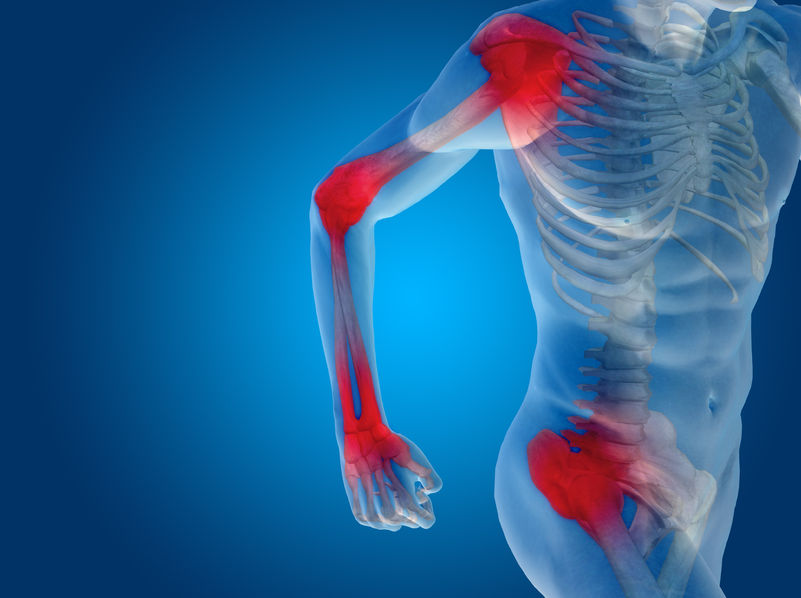
Pain!
One of the BIG topics in pharmacy and health care today is pain.
About 20 years ago, the American Pain Society (APS) introduced the idea of “pain as the fifth vital sign”. (The other vital signs are blood pressure, heart rate, breathing rate and body temperature.)
Health care providers started monitoring the fifth vital sign, usually using a scale of 0 to 10, with 10 being the worse imaginable pain. Pain was largely assessed by taking the patient’s word about the severity of their pain. Accreditation organizations started looking at how well providers were treating pain, and provided encouragement to aggressively treat pain.
Of course, the purpose of considering pain as “the fifth vital sign” and treating pain adequately was to improve patient care, and many patients have benefitted from increased use of pain relieving drugs. Unfortunately, more progressive pain treatment also contributed to some unintended consequences.
If you have monitored the news recently, you have likely seen something related to:
- too many people get prescriptions for pain medications;
- too many people take pain medications;
- too many people become addicted to pain medications;
- too many people die as a result of prescription pain medications.
The pharmacy profession and society have begun to respond to the problem. Many states have made naloxone – an antidote to opioid toxicity – more readily available to patients and their families. Patients on opioids have slowed breathing and can “forget” to breath. Naloxone can temporarily reverse this and save a patient’s life.
Most states now have prescription drug monitoring programs for controlled substances. These programs allow pharmacies to check on how frequently patients are obtaining prescriptions for opioids and identify patients who are visiting multiple prescribers to obtain prescriptions.
Many community pharmacies now more closely monitor the dosages that patients are receiving for noncancer pain; those prescriptions for higher doses of opioids are checked with the prescriber and patients are encouraged to begin tapering their dosage over time.
One of the concerns now (also known as the next unintended consequence) is the increase in heroin use, presumably by patients driven out of the healthcare system by these strategies to decrease the legal use of opioid pain relieving drugs.
I spoke at length with a fellow from the American Chronic Pain Association about pain treatment in the US; the group provides resources for patients, prescribers and pharmacists (link below).
The answer to the issue is greater involvement of prescribers and pharmacists to help patients balance the right kind of pain relief with other factors to optimize the ability of patients to function and interact with others.
If you are in pain, talk to your prescriber and pharmacists about your medications and options.
Sometimes it is a better choice to experience some pain so that you can still get around and talk coherently with others. Your prescriber and pharmacist can help you make the best decisions for you. It is important to take good care of your health.











