The Federal Drug Administration (FDA) approved two new cholesterol lowering medications in February of 2020. These medicines are part of a brand-new class of medication and work differently than the cholesterol medicines that have been available previously.
You might be wondering, why do cholesterol levels matter so much? Do you think of cholesterol as a bad thing? Associate it with dieting? Learn more about cholesterol here.
The truth about cholesterol is that cholesterol itself is not a “bad” thing. Your body actually needs cholesterol to function properly. Cholesterol helps your body make hormones and helps with digestion. Your body makes cholesterol in the liver, and it also comes from the foods you eat.
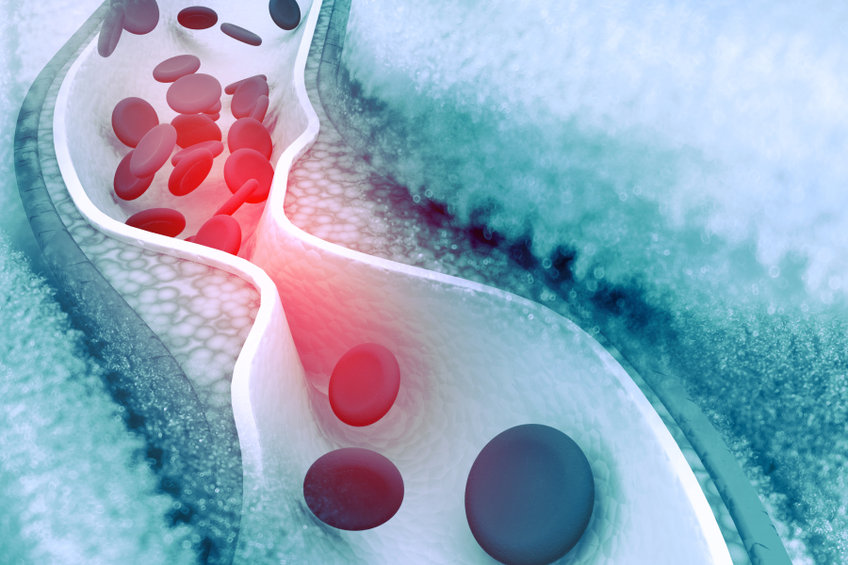
However, cholesterol can cause problems if it builds up in the arteries, which makes the arteries more narrow and less flexible (also known as atherosclerosis). If a blood clot formed in one of the narrow, hardened arteries, it could block off the blood supply to the heart or brain and lead to a heart attack or stroke.
The medical term for “bad” cholesterol is low-density lipoprotein (LDL) cholesterol and “good” cholesterol is called high-density lipoprotein (HDL) cholesterol. High levels of LDL, or “bad” cholesterol has been linked to heart attacks and strokes, thus medications are used to lower LDL levels and reduce the likelihood one of these events may occur. In addition, if someone taking a cholesterol-lowering medication does have a heart attack or stroke, these medications also can help decrease the severity of the event. They are also used after a heart attack or stroke to prevent a recurrence.
The preferred, and most common, medication class for lowering LDL cholesterol is the “statin” (or HMG-CoA reductase inhibitor). Examples of “statin” medications are atorvastatin (Lipitor®), rosuvastatin (Crestor®), simvastatin (Zocor®), and pravastatin (Pravachol®). These medicines are considered the go-to (or first-line) for lowering LDL cholesterol. When someone has had a stroke or heart attack in the past, medical guidelines recommend high-dose (or high-intensity) atorvastatin or rosuvastatin. However, sometimes people cannot tolerate taking these medicines or are on the highest tolerable dose of a statin and their ‘bad’ cholesterol is still high. In these cases, your healthcare provider might want you to try a new cholesterol lowering medication called Nexletol® or Nexlizet®.
Nexletol® and Nexlizet® contain a medication called bempedoic acid. Nexlizet® also contains a second cholesterol medication called ezetimibe, which also is found in the brand name drug Zetia®. Nexletol® or Nexlizet® is one tablet taken once daily to help lower bad cholesterol. It may be taken with or without food. Your provider should check your cholesterol levels eight to twelve weeks after starting the medication.
One warning included in the drug approval includes the possibility of increased blood uric acid levels. Your healthcare provider should monitor your uric acid levels while taking this medication. Another warning upon drug approval was the risk of tendon rupture or injury. During drug studies, tendon rupture occurred in 0.5% of people taking the active drug compared to 0% in those taking the placebo. This medication is not recommended in pregnancy or breastfeeding.
If you have had a stroke or heart attack in the past, are already taking a statin medication, and your bad cholesterol is still high, talk with your healthcare provider to find out if Nexletol® or Nexlizet® is right for you. If you have familial hypercholesterolemia, these medications also may be right for you. Talk with your healthcare provider.
Save up to 80% on the cost of your prescriptions at your local pharmacy with EasyDrugCard.com. Download your free drug card and begin saving today.
Resources:
https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/211616s000lbl.pdf